
Interest in regenerative treatments continues to grow as patients seek solutions that support healing without relying on synthetic substances. Discussions around PRF and PRP often arise during consultations for skin, hair, joint, or dental concerns. Both options use platelets from a patient's own blood, which creates trust but also raises questions about how they differ. Preparation methods, healing timelines, and treatment goals separate these therapies more than many people expect. Clear explanations help patients feel prepared before making decisions that affect comfort, recovery, and results.
Platelet therapy refers to medical treatments that concentrate platelets to stimulate natural repair. These approaches rely on growth factors already present in blood. Clinics offering PRF and PRP often describe these treatments as biologically driven rather than chemically enhanced. Understanding these fundamentals creates clarity before comparing specific options.
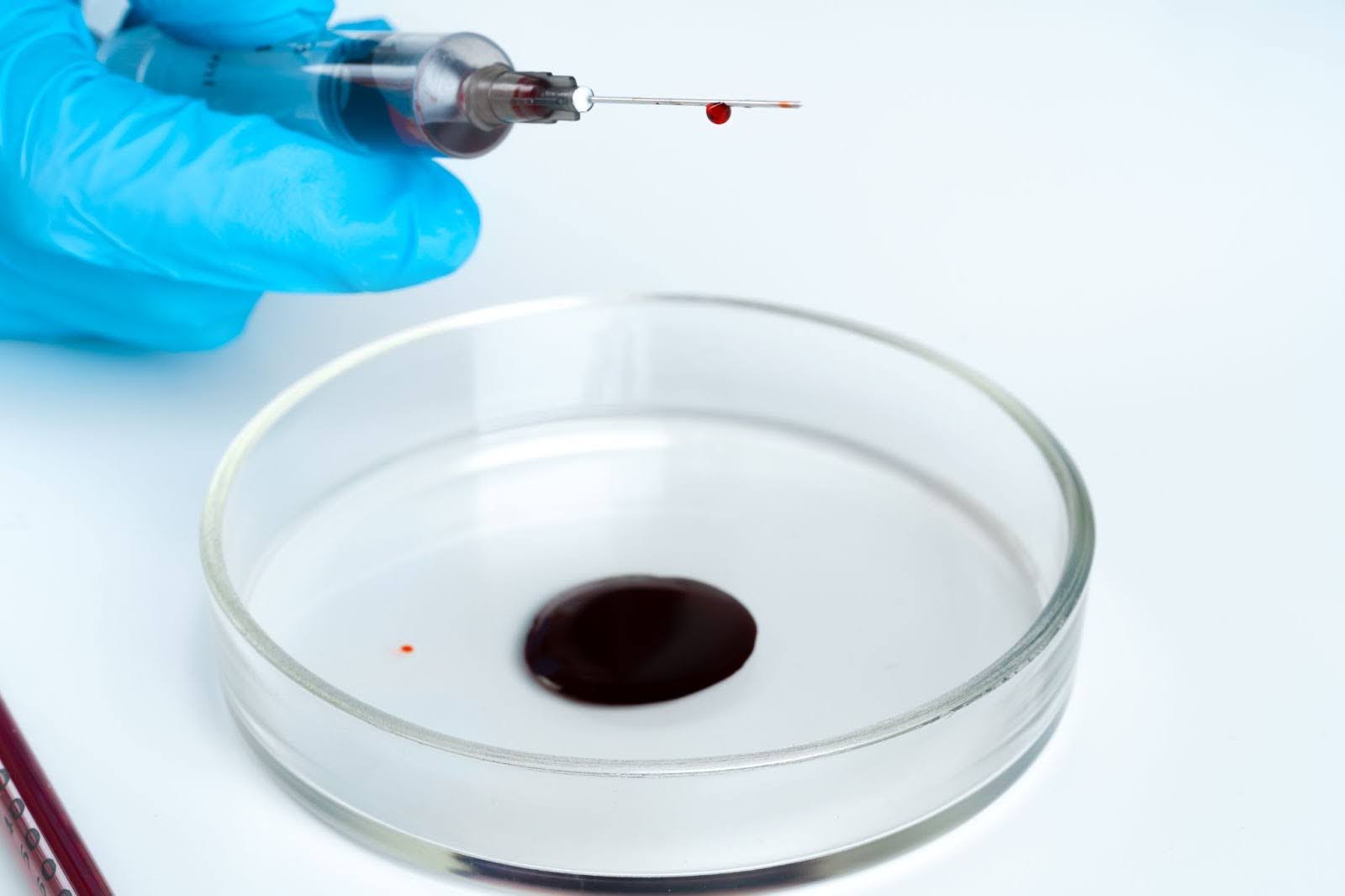
Platelets act quickly when the body senses tissue damage. These cells release growth factors that regulate inflammation and support repair. This coordinated response helps tissues rebuild in an organized way. Concentrating platelets increases the strength of these signals at targeted sites. This localized effect reduces unnecessary stress on surrounding tissue. Clinics favor this approach because it works with the body's existing systems.
Normal blood contains platelets in balanced amounts. Platelet therapy increases their density at specific locations. This increased concentration enhances intercellular communication. Stronger signaling improves tissue response during healing. Treatment outcomes depend heavily on this biological intensity. Providers adjust protocols based on treatment goals.
PRP stands for platelet-rich plasma, a liquid platelet concentrate derived from blood. This therapy gained early recognition in sports medicine before expanding into aesthetics and dentistry. PRP delivers growth factors rapidly to areas that need stimulation. Providers often recommend PRP when a faster biological response is appropriate.
PRP preparation starts with a routine blood draw. The blood spins in a centrifuge at high speed. This process separates platelets from other blood components. Anticoagulants prevent clotting during preparation. The final PRP remains liquid and injectable. Most clinics complete this process within thirty minutes.
PRP treatments usually involve targeted injections. Some providers apply PRP during microneedling sessions. Patients may feel brief pressure or mild discomfort. Sessions typically last under an hour. Downtime remains minimal for most treatment areas. Clinics often allow same-day return to regular routines.
PRP is widely used for joint and tendon issues. Sports medicine clinics rely on PRP for the treatment of overuse injuries. Aesthetic providers use PRP to improve skin tone and texture. Hair restoration programs apply PRP to support follicle health. Dental practices integrate PRP into surgical care. These applications reflect patterns seen in recent clinic data.
PRF stands for platelet-rich fibrin, an advanced form of platelet therapy. This option differs from PRP in structure and timing. PRF forms a fibrin matrix rather than remaining liquid. Providers often choose PRF when sustained healing support is desired.
PRF releases growth factors gradually over several days. This slow release supports extended healing phases. The fibrin matrix acts as a scaffold for tissue repair. This structure stabilizes platelets at the treatment site. Many providers report longer-lasting results with PRF. These findings align with current regenerative medicine research.
Dental clinics frequently use PRF during implant and bone graft procedures. Oral surgeons value its stability during healing. Aesthetic practices apply PRF under the eyes and in facial rejuvenation. Hair restoration clinics also incorporate PRF protocols. Wound care specialists explore PRF for complex healing cases. Use continues to expand as experience grows.
The PRF and PRP comparison focuses on structure, timing, and biological response. These differences influence how treatments perform after application. Understanding them helps patients set realistic expectations. Providers often explain these contrasts during consultations.
PRP remains liquid after preparation. PRF forms a fibrin-based matrix. PRP releases growth factors quickly. PRF releases them slowly and steadily. This timing affects healing duration. Clinics match structure to treatment goals.
PRP stimulates rapid early healing. PRF supports prolonged regeneration. Acute conditions may benefit from a faster response. Chronic issues often need sustained support. Healing timelines vary by condition. Providers consider tissue type and severity.
PRP often requires multiple sessions. Maintenance treatments help preserve results. PRF may reduce session frequency. Extended activity supports durability. Scheduling needs differ between options. Cost planning also varies.
Patient biology plays a direct role in how PRF and PRP perform after treatment. Platelet therapies depend on the quality of a patient's own blood rather than a standardized product. This biological variability explains why results differ even when protocols appear identical. Clinics that recognize these differences tend to deliver more consistent outcomes.
Platelet concentration and activity differ from person to person: age, hydration, and metabolic health influence platelet responsiveness. Chronic inflammation can reduce the effectiveness of growth factors. Certain medications may affect platelet behavior. This individual variability shapes how PRF or PRP performs after injection. Providers adjust expectations based on these biological factors.
Baseline inflammation changes how tissues react to platelet therapy. Elevated inflammation may blunt early PRP results. PRF often performs better in these cases due to its gradual release of growth factors. This sustained signaling supports steadier tissue repair. Clinics frequently observe this pattern during follow-up visits. These observations align with trends reported in clinic-level outcome tracking.
Personalized protocols account for biological differences upfront. Providers may adjust spin time or treatment intervals accordingly. Treatment areas also influence product selection. A tailored approach reduces unpredictable outcomes. Patients benefit from realistic timelines and clearer expectations. This personalization separates experienced clinics from standardized protocols.

Patient experience influences satisfaction and compliance. Both PRF and PRP involve minimally invasive procedures. Sensation and recovery vary slightly between options. Clear communication improves comfort.
PRP injections feel similar to routine injections. PRF may feel firmer due to consistency. Providers often use numbing agents. Discomfort usually remains brief. Anxiety decreases with a proper explanation. Patient feedback guides technique adjustments.
Mild swelling or redness may occur. PRP reactions often resolve quickly. PRF swelling may last slightly longer. Most patients resume daily activities soon. Exercise restrictions remain minimal. Aftercare instructions support healing.
Preparation technology directly affects the quality of PRF and PRP before treatment begins. Centrifuge design, speed, and timing influence platelet separation. Minor technical differences change growth factor concentration. Clinics that control these variables achieve more reliable results.
Centrifuge speed determines how blood components separate. High-speed spinning creates liquid PRP with rapid-release properties. Lower speeds allow fibrin formation for PRF. Timing affects platelet integrity during processing. Inconsistent timing reduces biological effectiveness. Experienced clinics follow precise protocols for consistency.
Medical-grade centrifuges provide controlled separation. Lower-quality equipment may produce uneven platelet concentrations. Variability leads to inconsistent clinical results. Clinics investing in advanced systems reduce these risks. Equipment choice reflects commitment to quality care. Patients rarely see this difference but experience its effects.
Provider technique influences product handling after centrifugation. Delays reduce platelet activity. Improper transfer affects concentration. Training improves efficiency and consistency. Experienced teams adapt protocols to treatment goals. This expertise often determines long-term satisfaction.
Selecting PRF or PRP depends on medical needs and personal goals. Providers evaluate tissue type and healing capacity. Lifestyle factors also influence decisions. Professional guidance ensures alignment.
PRP suits patients seeking texture improvement. PRF benefits delicate areas needing gradual support. Skin thickness affects selection. Aging patterns guide recommendations. Providers customize plans after evaluation. Personalization improves satisfaction.
PRP supports inflammation control and tissue repair. PRF aids bone integration and stability. Dental clinics often favor PRF during surgery. Orthopedic practices may prefer PRP flexibility. Specialty goals influence choice. Experience shapes protocol selection.
PRP may require repeated visits. PRF often reduces appointment frequency. Work schedules influence preferences. Budget planning matters for long-term care. Healing timelines affect social plans. Clear discussions support informed decisions.
PRF and PRP rely on autologous blood sources. This approach reduces allergic reaction risk. Safety depends on training and equipment. Reputable clinics follow strict protocols.
Swelling and bruising may occur. These effects resolve within days. Infection risk remains low with sterile technique. Pain typically stays mild. Providers monitor response closely. Patients receive guidance on warning signs.
Centrifuge quality affects results. Timing matters during preparation. Experience improves consistency. Training reduces variability. Patients should ask about credentials. Transparency builds trust.
Platelet-based treatments work best when they reflect a patient's specific needs rather than a one-size approach—factors like healing capacity, treatment area, and desired outcomes shape which option delivers the most value. A thoughtful consultation helps translate medical insight into a plan that feels practical and realistic. When expectations align with the biology behind the treatment, confidence replaces uncertainty, and results tend to follow.
Stay informed with thoughtful, expert-driven content on regenerative skin aesthetics by visiting the Naples Laser & Skin Aesthetics blog and expanding your understanding.
%402x.svg)

.png)
3641 10th St N Suite B, Naples, FL 34103